Social Determinants of Health
There are many technical, operational and economic barriers to making meaningful progress when it comes to addressing needs in regard to social determinants of health (SDOH) and health equity (HE). Contributing factors include lack of funding, inefficient information sharing among the stakeholders, poor situational awareness and cultural barriers. SDOH encompasses the conditions and circumstances in which individuals are born, grow, live, work, and age, all of which have a profound impact on their health outcomes. Health equity, on the other hand, refers to the principle of ensuring that every individual has the opportunity to attain their highest level of health, regardless of social, economic, or other factors that could potentially create disparities in health outcomes.
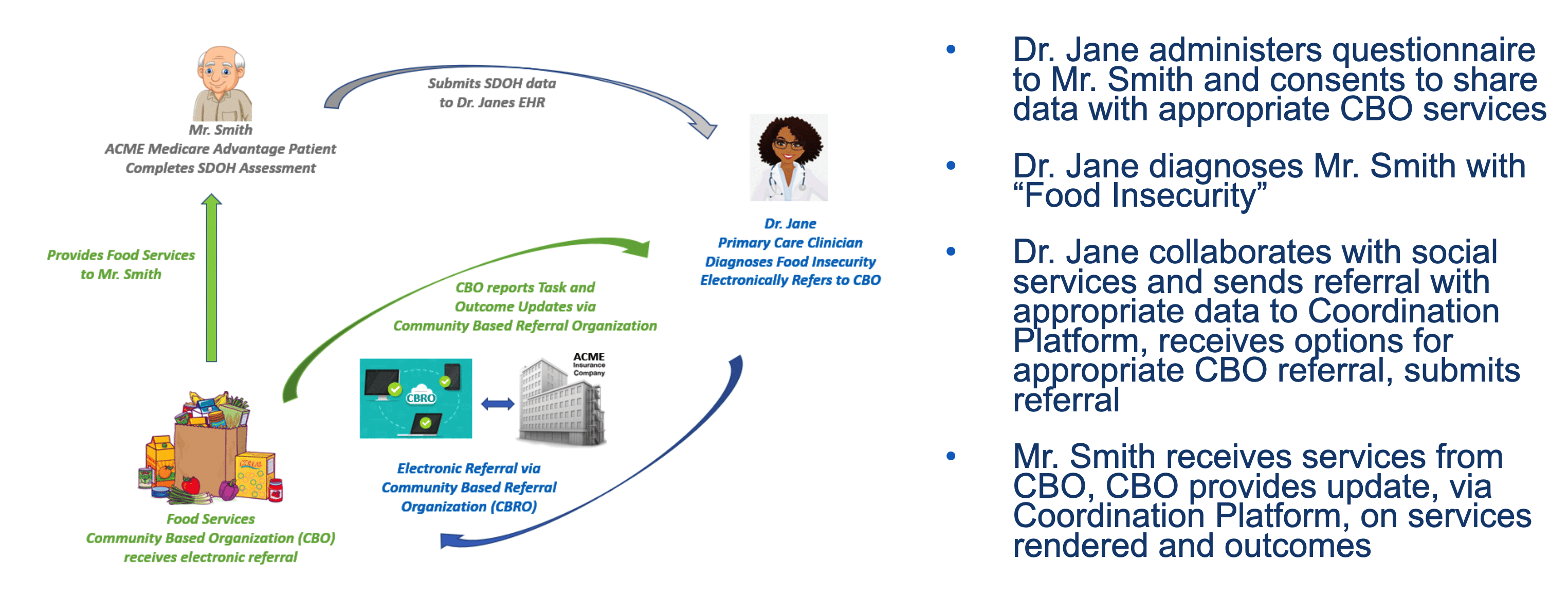
Information sharing between the healthcare team, community based service organizations (CBOs) and patients is key to enabling the effective management and integration of SDOH concerns into a holistic plan of care.
Electronically communicating patient specific SDOH and HE information can improve:
- Identifying health concerns using standardized codes and HL7 messaging to improve transparency and support shared care planning, CDS and analytics.
- Referral management to appropriate social services through community based organizations.
- Shared individualized care plans that incorporate input from the patient, healthcare provider and community services provider.
- Outcomes analysis to assess the effectiveness of different types of interventions.
- Different types of decision support ranging from eligibility for certain services to matching patients with the most appropriate types of interventions needed at the right time when they most need them.
- Identifying and addressing HE disparities that would be very difficult to measure without the collection of unbiased and timely data.
Learn more about how SDOH factors into our Services and Solutions:
Today Elimu Informatics is addressing information sharing through it’s participation and contributions to several large interoperability efforts that have been in development since 2017:
- The FHIR Gravity SDOH Clinical Care project is a standards development effort focused on facilitating efficient communication of referrals for social services between health care providers and community based organizations. This project is currently supported by Civitas, CMS, ONC and a large community of community based organizations and health care providers. The Gravity Team includes the AMA, Elimu Informatics, Lantana, and the core Gravity SME / terminology standards team working together to continue to refine this standard with feedback coming from several large pilot implementations that are currently underway. To learn more please visit:
- Gravity Project Home: https://confluence.hl7.org/display/GRAV/The+Gravity+Project
- Gravity Pilots: https://confluence.hl7.org/display/GRAV/Pilots+Workstream
- FHIR Gravity SDOH Clinical Care Implementation Guide (the standard): https://build.fhir.org/ig/HL7/fhir-sdoh-clinicalcare/
- The FHIR Electronic Long-Term Services and Supports (eLTSS) Implementation Guide is a standard focused on the sharing of a patient facing care plan that addresses needs related to long term services such as in-home assistance, SNF and much more.
- The FHIR MCC eCare Plan Implementation Guide is a standard that supports multiple conditions management and incorporates participation from the patient, the physician, social worker, other supporting health care providers and much more. It’s not SDoH specific but supports both Gravity and eLTSS.
To date, Elimu Informatics has contributed to HL7 FHIR standards development that supports interoperable capture of Social Determinants of Health needs, appropriateness screening for community based services, descriptions of referral services and tracking of patient outcomes. Our development team has also participated in a CMS Connectathons that illustrates how interoperability standards and approaches can support closed-loop referrals between clinical care teams and community-based organizations. Our team provides professional services through the Gravity Pilots Affinity program on how to integrate the ecosystem of health systems, community based organizations and public health agencies to support patients with SDOH needs. Elimu’s SMART-on-FHIR Apps can be a vehicle for reducing the burden on IT organizations wishing to deploy maintainable solutions that integrate seamlessly with clinical workflow. Below is a graphic illustrating how apps can support clinicians assessing SDOH needs, making referrals to Community Based Organizations (CBOs) via coordinating platforms, and receiving updates on services rendered.
Additional Background on the Importance of Social Determinants of Health (SDOH)
Understanding the Role of SDOH:
SDOH comprises a wide range of factors, including socioeconomic status, education, employment, housing, access to healthcare, and the social and physical environment. These factors significantly influence an individual's health, even more so than traditional healthcare interventions. For instance, a person's access to nutritious food, safe housing, and quality education can be more critical to their overall health than medical treatment.
- Socioeconomic Status: Income, education, and occupation are major determinants of health. People with higher socioeconomic status tend to have better access to healthcare, nutritious food, and living conditions that promote health.
- Housing and Neighborhood: Living in safe, stable, and clean housing, as well as residing in neighborhoods with access to green spaces and community resources, can positively impact health.
- Access to Healthcare: Availability and affordability of healthcare services, as well as health insurance coverage, influence an individual's ability to seek timely medical care and preventive services.
- Social Support Networks: Having a strong social support system can mitigate the adverse effects of stress and promote overall well-being.
-
- Employment Conditions: Job security, workplace safety, and access to paid leave can significantly impact an individual's physical and mental health.
The Role of Health Equity:
Health equity seeks to eliminate health disparities that arise from socioeconomic, racial, and other systemic inequities. It recognizes that not all individuals have equal access to healthcare and the same opportunities for good health. Achieving health equity involves addressing these disparities and promoting fairness in healthcare delivery and outcomes.
- Reducing Health Disparities: Health equity initiatives aim to narrow the health gaps between different populations. This may involve targeted interventions to address the unique needs of marginalized communities.
- Providing Culturally Competent Care: Understanding and respecting cultural differences in healthcare practices and beliefs is essential to ensure that care is accessible and acceptable to all.
- Policy and Advocacy: Advocates and policymakers work together to identify and rectify systemic barriers to health equity, such as discriminatory policies and practices.
- Data Collection and Analysis: Collecting and analyzing data by factors such as race, ethnicity, and socioeconomic status can reveal disparities and guide evidence-based strategies to promote health equity.
- Education and Outreach: Raising awareness about health disparities and promoting prevention and early intervention can empower individuals to take control of their health.
In health management, addressing SDOH and promoting health equity are integral to improving population health outcomes and reducing healthcare costs. Healthcare organizations, providers, and policymakers are increasingly recognizing the importance of integrating these principles into their practices. By acknowledging the role of SDOH and striving for health equity, we move closer to a healthcare system that values all individuals equally and ensures that they have the opportunity to lead healthy lives, irrespective of their background or circumstances.